Similar symptoms cause confusion between COVID-19, seasonal illnesses
Knowing the symptom differences of respiratory illnesses can better help identify and diagnose an affliction.
December 12, 2022
As COVID precautions are lifted and fewer masks are being worn, students cough up and spread unknown infectious particles alongside classmates, causing a germy epicenter to form from frequent close-contact interactions in classrooms.
“I have been healthy for almost a whole month after diagnosing myself when I was coughing with a fever over 100 degrees,” sophomore Trent Saben said. “I chose to stay home after being ill over the weekend. During this time I have felt very sore and could not catch a break without feeling some type of internal pain. I have felt all types of pain ranging from bone aches to throat problems.”
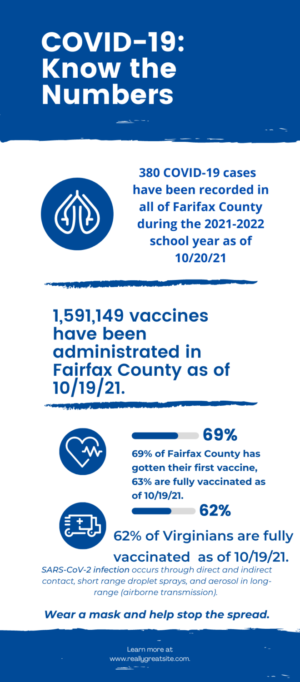
According to the Centers of Disease Control and Prevention (CDC), COVID-19 related visits for pediatric patients have increased during the start of this year’s fall and winter flu season as compared to during the pandemic. An increase in hospitalizations have been attributed to the dangerous consequences of coronavirus and flu symptoms, including severe long term damage to a variety of organs for coronavirus, and inflammation of the heart and muscles for the flu.
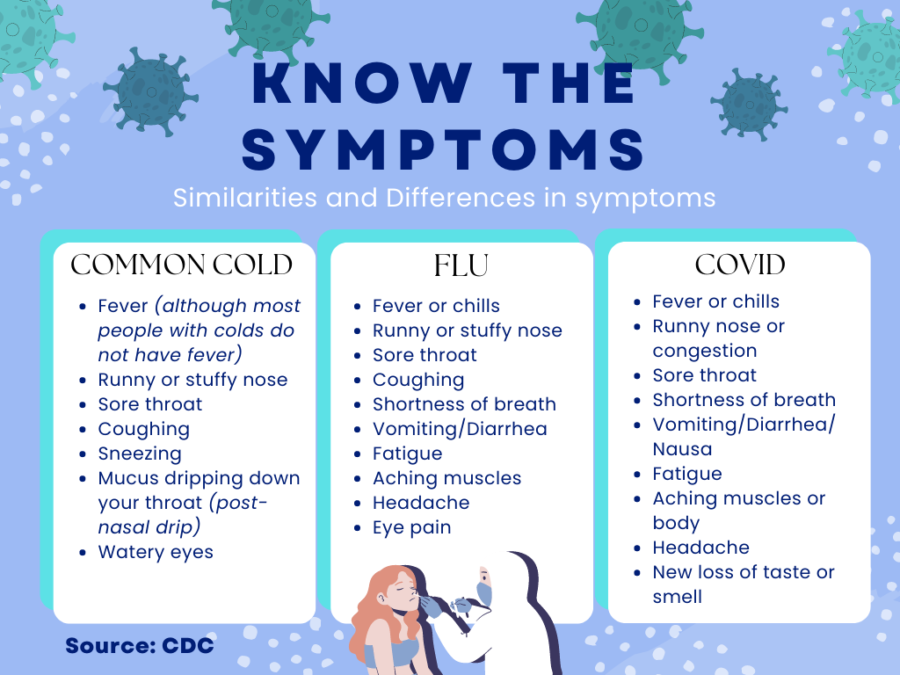
Although coronavirus has been in the limelight lately, these symptoms of seasonal illnesses such as the common cold or allergies have blurred the lines on how to diagnose the actual affliction. Unsure of what sickness they have caught, increasing ambiguity and potential danger put students and staff at risk.
Cold symptoms are more mild and can be easily treated with over the counter cold and flu medicine, while COVID-19 typically comes with muscle and body aches, alongside gastrointestinal symptoms (upset stomachs, diarrhea, nausea and vomiting) that don’t typically happen with a cold, but can be a sign of infection.
“I think that we’re potentially going to get back to taking more preventative measures from the influx of viruses this winter, it’s not such a good outlook,” Nursing teacher Cynthia Holland said. “I’m not saying to go out and wear a mask right now, but to stay open minded to that possibility, because it’s not always about you, it’s the people around you. We all know that people have issues with their ability to fight infections.”
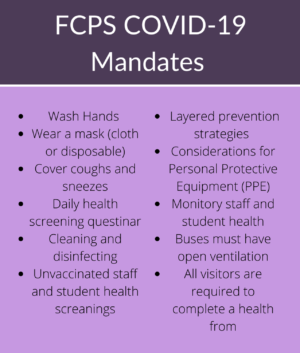
According to the CDC, the weekly average of reported cases of COVID-19 have decreased by 30.9% from the previous spike of 57,564 cases in Dec. 2021, to 39,803 cases as of Oct. 19, 2022. Although the number of reported cases has decreased, the heightened transmission risk factors associated alongside new sub-variants of COVID-19 (named BQ.1 and XBB) continue to rapidly evolve. With these new variants rising, safety precautions continue to be practiced by students and staff such as using face masks, covering sneezes or coughs with arms, washing hands and keeping a safe distance from people are recommended to prevent the spread of germs.
“It’s important to protect peers from getting sick so that they will not have to go through the same troubles as you, so that they won’t spread it to others like a domino effect,” Saben said.
According to the CDC, to prevent further spread of the diseases, isolating for five days at home is recommended after testing positive for COVID-19. Contact a healthcare provider for additional guidance if necessary.
“Twice just this year, I have seen students come in who are not feeling well, have missed questions on assessments, have not been able to engage in their learning [without their] heads down, struggling to stay focused on tasks they normally would function at,” chemistry teacher Shaundra Riggleman said. “If a student is feeling unwell to the point that it impairs their ability to actively engage in material, they should be at home resting.”
Respiratory viruses such as COVID-19 and flu symptoms are commonly mistaken for one another, or could be the result of co-infection, which is having multiple viruses at once.
According to the Cleveland Clinic, symptoms unique to coronavirus can take longer to show and stay infectious on body systems outside the lungs, while typically symptoms go away for flu once the virus leaves the lungs. Loss of taste, smell, vomiting and diarrhea are common symptoms among respiratory viruses.
Preventative measures can be taken against COVID and other respiratory illnesses by maintaining healthy habits, which improve immune responses and provide essential nutrients for bodily functions. By getting the recommended eight hours of sleep, adding fruits and vegetables to one’s diet or taking dietary supplements that include sources of Vitamin C, Vitamin D and Zinc help provide vital antioxidants, vitamins and minerals that strengthen the immune system. Studies show a higher risk of COVID-19 and respiratory tract infections are correlated with low vitamin D levels.
“Get plenty of rest, eat well, exercise and in general, also take care of your mental health- that’s part of it too,” Holland said. “The healthier you are, the more tools you have in your arsenal to fight it when it does hit you.”